Speech Therapy and Parkinson’s Disease
Andrea Malsom @myvoicetherapy and Mark @MarkinthePark21
Strength in the Face of Parkinson's - Podcast Episode 1
If you are on social media and connected in any way to the Parkinson’s community, chances are you have seen Mark’s content at @MarkinthePark21. It is even likely that he introduced you to the social, engaging, and supportive Parkinson’s community on Instagram and TikTok. He is a wonderful advocate for those with Parkinson’s and shares how he is handling his own personal diagnosis of Young Onset Parkinson’s Disease. His humor, kindness, and inclusion is so powerful and I am honored that he volunteered his time to interview myself during my first podcast interview.
Please enjoy our discussion through my modified-for-blogging show notes, below,
or through the recording of Strength in the Face of Parkinson’s, Episode 1 wherever you listen to podcasts.
Introductions
Andrea: Hi, I'm Andrea Malsom and I'm here with Mark. I was sharing on Instagram how I was going to lecture at Gray Strong Foundation about speech therapy and Parkinson's. And he was messaging saying that he was bummed that he couldn't make it and that maybe we should do an interview about what speech therapy is.
Mark, you wanna tell us a little bit about yourself?
Mark: Yes! In February I had the anniversary of my one year date of my diagnosis from Parkinson's disease, which I felt was a significant date because I had made it through one year.
And my first year in diagnosis, so to speak has been such a learning year. It's been such a year of growth reaching out, trying to understand. and try and understand the disease that I have or the condition that I have and understand the remedies and the things that can help and those things.
And there there's such an individuality to Parkinson's that there's a lot to learn because it affects so many different people, different ways. And one of the things as we discussed was, was speech therapy, something I hadn't even really gone down the road on, which is why. Your sessions were interesting to me.
As I try and learn and grow in my knowledge of Parkinson's and what helps Parkinson's people. And so that is one of the significant things I did in my first year with Parkinson's was just trying to learn. And so entering year two, trying to expand on that knowledge. And that was part of this conversation.
In trying to understand what you do as a speech therapist, speech pathologist, and working with Parkinson's people. One of the things I was struck by was that I really didn't know what you could do for me or somebody with Parkinson's because I don't really know, like the old saying you don't know what you don't know.
And that's kind of what I felt like when hearing about your sessions, I thought, why, why, why would I need this?
Becoming a Speech Pathologist
[00:02:06] Can you tell me a little bit more about your background and your training and what you've been?
Andrea: Yeah, that kind of goes hand in hand on why a speech therapist would land in this kind of specialized position to help those with Parkinson's disease.
I'm from Michigan, the Metro Detroit area. I always loved the one-on-one tutoring and kind of being a counselor. I did my undergraduate schooling at Western Michigan University and that's where I met my husband, that's where I got into the speech pathology department. It was a perfect mix of my interests and my personality as a helper. And then my graduate schooling at Wayne state University, which is Detroit area.
Through speech pathology, I realized that I like the medical, adult side. I was passionate about helping adults regain what they had lost and what they were very motivated on returning back to. I really liked learning about the things that we didn't know, like:
How do we breathe? Like what turns that button on to breathe and where do we breathe from? That's where the voice comes from the, the sound articulation that we have, the emotion. And so if any of that pathway is impaired, how do we overcome it? It was like a puzzle to me.
The brain can be impaired and impact speaking, communicating, thinking, and swallowing in a different way than if there was like a muscle injury.
And the rehabilitation is different depending on the side of injury and the, the cause for that change. Those adults were so motivated to return back to the, their job or the way that they used to talk or back to their foods that they like to enjoy.
And that was that's different in my view than if I was a speech pathologist with children. So it, it just, I, I kept heading that direction. I got jobs in hospitals and nursing homes and long term cares and then I became an outpatient speech pathologist and I was able to add another certification, start my own practice, and really put my whole heart into supporting people.
How Parkinson’s Disease Treatments Differ
[00:04:34] Mark: Well, you, you just said so much there, and that is fascinating, but one, one of the things you, You mentioned the therapy is different from somebody that has a traumatic head injury, as opposed to somebody that has Parkinson's and a lack of dopamine. There's two different methodologies there, right? There's two different. Ways you approached that, right?
Andrea: Absolutely.
It's very different than the slower progress that with someone that has stroke even post concussion syndrome, head injury.
Sometimes it takes a long time for those, to recover and get back to their normal self. With Parkinson's, it's really rewarding, because you can reach these levels of clarity so much quicker.
And that was another reason why I fell in love with the treatments for Parkinson's disease, I can get the voice stronger the first day I meet them like it's just, it's amazing that to see that.
And the challenge is different. Parkinson's does not allow them to realize if they're being loud enough. Parkinson's gets in the way and you have to break through Parkinson's barrier every time you go to speak and that's very challenging and you have to learn a new way of regulating your voice.
Do I need Speech Therapy for Parkinson’s?
[00:05:48] Mark: When somebody realizes that they need to come to a speech therapist and, and, and get your, your service, would you say that most of the time they're aware of it or did somebody bring it to their attention? I mean, how does, how does somebody know?
Andrea: Good question.
Mark: I'm just thinking of a Parkinson's patient that may be told by their spouse that they're not speaking as loudly as they used to, or, you know, along those lines. So how do they normally come to the realization they need speech therapy?
Andrea: They need the education and they need that time to take on that information.
And talk about:
Are they experiencing people not hearing you?
Have they had a lot of people ask them to repeat themselves?
Has the world developed a “hearing loss” in their life?
Do you have drooling and coughing and choking?
I have to get through the feedback loop that's impaired by Parkinson's. We go through the whole process of let's try it out, let's do a video recording and then play it back and see the difference between when I had you just talk normally and then when I cued you to talk in a different way.
Another way that they come to me is that they're noticing changes. They they're noticing that their speech is either too fast or too slow that they can't understand themselves. Their family can't understand themselves and they just feel like their, their mouth is just moving way too fast.
But they still need all the awareness they need, they need all the education and they need that time to take on that information and kind of guide them through that process. So it's a, it's a mix like you said, there it's a mix of symptoms people experience Parkinson's differently. They, they experience speech changes differently.
90% of people that have Parkinson's disease will have a speech or swallowing change sometime in their progression but only a fraction of that get speech therapy.
Mark: That's a huge percentage. That's that's amazing.
Andrea: So it's, it's not even, you know, a, an acceptable amount that, that actually receive the help that they could benefit from.
And I'm really curious about how much the DBS the deep brain stimulation is impacting that process. Are they more aware of it because of the DBS? You know, how is that changing?
Mark: I'm learning more and more about that deep brain stimulation.
And I've noticed that there are some people that have deep brain stimulation implants still talk really, really fast. And I wondered about that. Is that something that, that DBS has, has helped already, but maybe hasn't helped if that makes sense. So that's interesting. That's an interesting variable to the Parkinson's whole situation. Interesting.
Trouble Swallowing for Parkinson’s Disease
[00:08:49] Andrea: And unfortunately, the swallowing changes that can eventually occur can cause the eventual passing of someone with Parkinson's. That can be supported by speech therapies efforts to change that course from happening.
Mark: Absolutely. Yeah. I know. I had looked at a website. There was something listed like 70% of people pass from you mentioned the aspiration.
Andrea: Aspiration pneumonia, which is the food and liquid going the wrong way and settling in your lungs and then staying there and then developing an infection. And that aspiration pneumonia is related to swallowing change or coughing or choking over time. That's 70% of those with Parkinson's disease pass away from aspiration pneumonia.
Mark: Wow. That's that's crazy. Now you mentioned earlier being able to even impact the types of food that people eat. Can you explain that a little more because I, I think this is kind of interesting.
Andrea: Yes, Speech Pathologists provide dysphagia treatment, which is trouble with swallowing. We identify if they're having change in swallowing, what's causing that change and how we can help them. Swallowing can be impacted by Parkinson's and helping them sometimes is changing the diet consistency, changing the utensils that they're using like a certain straw cup that slows the quickness of the drink.
And speech and swallowing exercises that really help their ability to be safe while eating and swallowing.
Mark: Right.
Andrea: And drooling suggests that the muscles around your mouth can't contain the saliva, or the food that might be leftover in there. It also might suggest that there's a loss of initiation of swallowing. You don't effectively swallow each time you do swallow something down.
[00:10:27] Mark: Wow. Yeah. It's one of those things. There was a thread there on social media and, and gagging and swallowing actually came up. And a number of us with Parkinson's we're discussing in that thread. How many of us find ourselves periodically choking or gagging? And, and I've been embarrassed by it because I'm, I'm over 50 years old. I should know how to swallow by now. Right. But yet in the last I would say in the last three years there's been issues.
And one of the things that I had read is that some of the non-motor symptoms of Parkinson's can actually set on well before the actual motor symptoms of Parkinson's. So in other words, before the tremor starts, other things can start happening. And I wondered about that was, was it the, the swallowing issues that I was experiencing part of this as an onset.
And I, I do know that my handwriting, so I get my little pen out here. My handwriting literally changed over maybe a year and a half before experienced my tremor. And I, I got really micro writing and I got to the point where I can, I have a really hard time writing at all anymore. And so I wondered if that gagging and swallowing issue was, was part of this.
Andrea: Yeah. And you know, maybe you were noticing small changes. And in what I've heard from my patients is that they notice the change in their swallowing early on with the diagnosis, but it hasn't gotten worse.
So it's kind of like, it's It it's kind of there and they they've accommodated for it.
Mark: True.
Andrea: They withdraw from certain foods and they don't realize what else that they can do. And they can work with speech therapy on that.
Mark: Right.
Andrea: Especially if they're having any voice changes because the voice exercises that we do, the really specific ones for Parkinson's disease, help with swallowing and help with the drooling.
Voice Therapy for Parkinson’s Disease and Swallowing Changes
Andrea: The research knowledge that we know is that your body has to use a lot of intent to be able to perform. We sit down and we perform vocal exercises, also breathing exercises, facial expression it's all connected.
And I guide you through this process to say, what does that feel like to you being loud? And if you're feeling the loudness coming from, your diaphragm, then you should be loud enough.
So where do you stand? With loudness rate of speech, hoarseness quality, facial expression, monotone pitch all those characteristics of communication.
And what happens when you're doing it in conversation?
What happens when you're doing it in reading?
What happens when I throw a motor task in there?
And what happens if I throw a cognitive task in there and then I identify, okay, what can we reach?
So if I give you a clue to do it this way are you able to hit that, that mark?
And the muscles are not injured, they're not cut. We just haven't been using them and you use it or lose it with these muscles. You can't see these muscles that well and you can't feel them that well but people can hear the change. They can hear the weakness.
Mark: Right. So the atrophy, just like any other muscle, right.
Andrea: Yeah. So over time we do exercises to build that up, but they have to be this intense exercise because that's what Parkinson's needs to be able to gain that kind of benefit from physical exercise.
Mark: Sure.
Andrea: Like we do a lot of voicing and exercises and practice while you're doing other tasks at the same time. And just trying to challenge your brain.
What does Speech Therapy for Parkinson’s Look Like?
[00:14:01] Mark: How long are you sessions?
Andrea: The sessions are about 50 minutes, to an hour. But the important part is, is that the frequency it's three times a week, three to four, depending on what program you use.
Mark: Wow.
Andrea: Three or four times a week for four weeks straight. And then you get that muscle strength up, you get that awareness going and then you're able to carry over on your own, doing your homework and be more aware of it by the end of the month.
Mark: That's that's you used the word intentional and I love that because yes, with Parkinson's, to your point.
You, you have to become intentional about a lot of things. Whether it's speech therapy, whether it's exercise, diet change, there's a lot of things that you have to do. And, and that's pretty intense when you're talking about 45 minutes to an hour, that many times that's, but, but it's like boot camp for speech therapy. Really.
Andrea: Yeah.
Connecting with Clients
[00:14:59] Mark: So when you think back on the, the people that you've worked with, is there a favorite story, somebody that you worked with that maybe stands out that you like here was a breakthrough that really brought a smile to me or that I really enjoyed seeing this happen along those.
Andrea: The first story that comes to mind is a gentleman he was in policy making for healthcare. And he had Parkinson's. We were able to connect a lot about where the healthcare world is going and kind of having these big conversations and it was just really, really wonderful to be able to to hear him and hold a conversation and he was able to do the board meetings with more success.
Sharing in the Joy
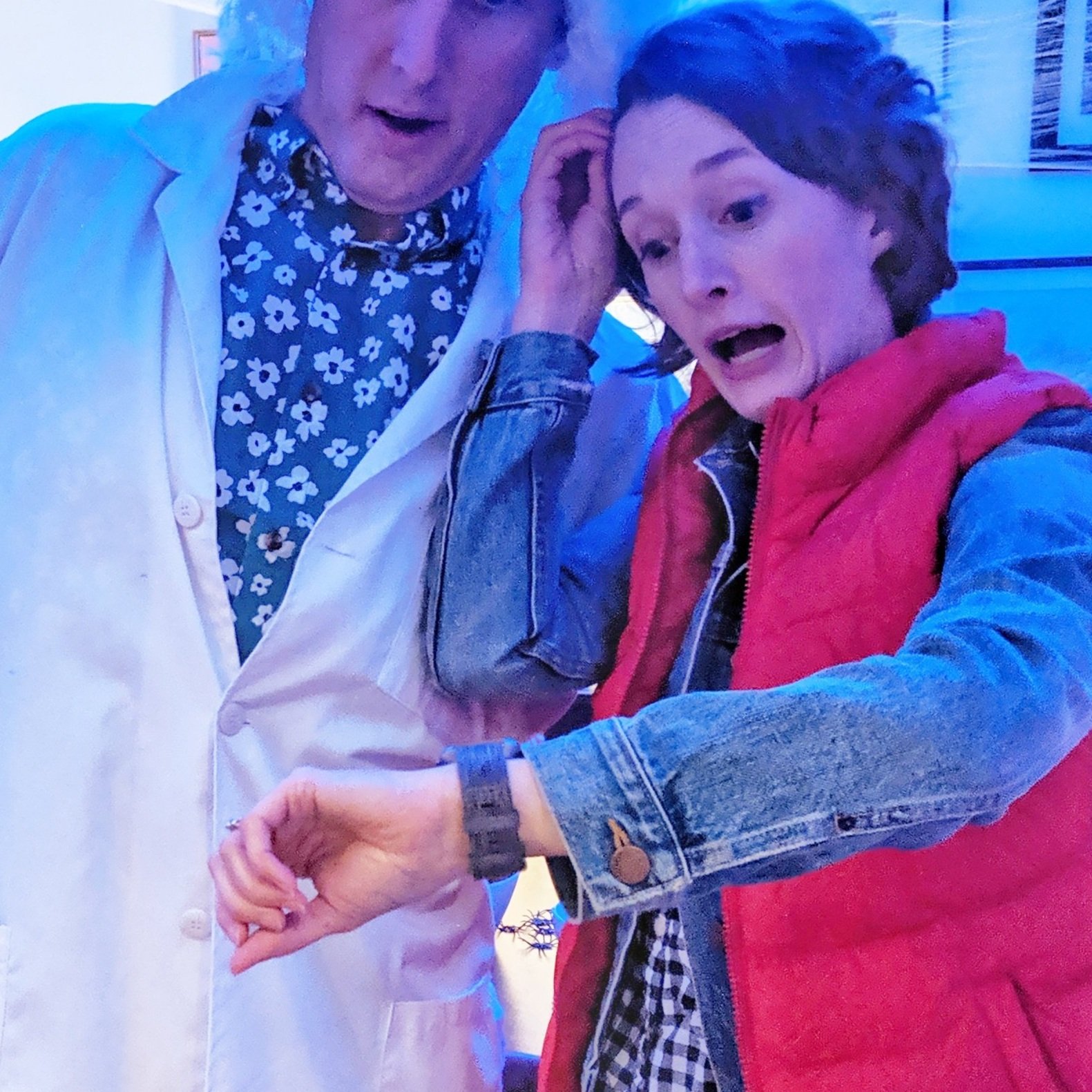
And the last day was Halloween and he showed up in Zorro with a cape. I showed him the photos for my Halloween party. And I was Michael J. Fox from back to the future.
I had the red vest and the jeans and, you know, the, the, the plaid shirt or whatever.
And he actually didn't do that well the last day. And I was like, what's, you know, what's happening here? Like you were so good with your voice. And he said he was he was really sad to stop our meetings. He really, really saw a difference when he had motivation to meet someone and have this connection. And he, he sounded devastated that he was stopping our service. So we brainstormed some other social events that he could continue doing and ways around this to help him.
And then also to talk to his neurologist. The, the mood changes that could be happening because of the literal brain changes in your brain as Parkinson's patient.
And then one more other story I had just, I, I have some really great clients that I worked with.
The other client was someone who was had kids in college, two girls in college and he was still working. He was a manager at a factory and we improved his voice and he did really well. His plan was to announce to his employees that he had Parkinson's disease and he wanted it to be the strong message. And he wanted to show them that he wasn't weak and he was still capable. But he wanted to do it on his own terms to share his, share that story beyond his family and into his career that he built. And he was able to do so because of speech therapy.
Mark: That is awesome. Boy, that's impacting some people in, in a tremendous way and I can I can just see you dressed up as Michael J. Fox looking for doc brown, Marty, you know, it just be great, you know, with, and you traveled back in time to be a Zorro.
Andrea: Yeah. It, it was good.
Social Isolation in Parkinson’s Disease
[00:17:33] Mark: Well, and you mentioned you helped him with his self isolation. So I mean, that's really going beyond speech therapy. That's the, that's the caregiver in you coming out? That is actually something I was talking with a friend of mine recently, I tend to be a social person.
I tend to enjoy being around people and I have had a tendency to withdraw and to be self isolating and some good friends of mine have been calling me out on that. And, you know, Hey dude, you need to do this. Right. And that's what friends do. And I love the fact that, you know, you went above and beyond the speech therapy to help this man with his isolation too, to make a plan, to give him. Some some things to think about to make sure he is not self isolating because it's not good.
Andrea: To acknowledge it, but also to say like, yeah, it could be the Parkinson's don't be so hard on yourself Michael J. Fox foundation had a lot of PDFs on apathy and delusions and the mental health side of things. I also kind of snuck it in there when they had to do their reading challenge. I gave them the, the PDFs of the, the nutrition ones And the DBS once and they had to read it out loud and, and learn a little bit about their diagnosis a little bit more. If, if you had Parkinson's apathy and withdraw, and then you also had loss of ability to maintain a conversation because you're flat in your voice and you are quiet and they don't wanna, you know, keep asking you to repeat yourself. Then those are two big bomb shells that kind of withdraw you from the society.
It doesn't have to be that way.
Mark: There you go.
Andrea: Yeah. That's I mean, that's why I love this, you know, the field that I'm in and then also the specialty that I found myself in it's. It's amazing to give them that connection. Like I got to know that gentleman, right. Both of them because you get to see them so often in a short kind of period of time, but they get to share your life and they, they get to find someone that can I actually hear them.
And it's kind of like the first exchange of that in a few years. And it's, they're just thrilled that it can happen again.
And it's surprisingly how many people in the area, but also nationwide are not aware of the connection of speech therapy and Parkinson's. So that's why I'm doing my service to get the word out that we need more people to be aware of this.
A Day in the Life of a Speech Pathologist
[00:19:52] Mark: Right, right. So, what is your current schedule? You're doing a lot of different things. I know you're doing some classes. What, what, what is your current schedule?
Andrea: So today I had a patient in person. I saw someone here in Kalamazoo. I traveled to her house and I was able to bring my tools.
I just have a little bag that I carry in, in her own setting. We talk about the things that she's interested in that she's used to.
And then I provide two different levels of the weekly class that's supported by the Parkinson's voice project. I've gotten some really excellent feedback and they say it's really nice to kind of see someone else in their same shoes, struggling and trying to overcome their voice changes with Parkinson's and that's excellent. That's just, just a free, free class. Kind of hard to call a class because it's like a support group in a way. But the prerequisite is that you do have to have speech therapy under your belt for Parkinson's.
Mark: You must compete that speech therapy first before going to that. Gotcha.
Andrea: Yeah, And then this afternoon I had a virtual client that I saw in Florida.
Mark: Yeah. The, the pandemic has brought about technology like zoom and other yeah. Things like that and normalized it, which in your case is probably a good thing because you can do this this way.
Andrea: I agree with you a lot more people are comfortable with it too, when they've had a doctor's appointment or a checkup virtually over the pandemic. And so, you know, it's not a big leap to therapy.
How to Find the Right Speech Pathologist Near You
[00:21:18] Mark: Sure. So if I'm wanting to get ahold of you for your services, how do I go about doing that? How am I gonna get in touch with you and say, I need some speech therapy?
Andrea: I have a free consult, a virtual call, on my website MyVoiceTherapy.com. It's a good way to get to know my services and figure out what the next step is, if it, if speech therapy is right. And then if you have a script, you can contact me on email, call me, or schedule your initial visit through my website.
There's also resources on my website, to learn about the different certifications. LSVT LOUD, which a lot of people know of the LSVT BIG. And the SPEAK OUT!, which is supported by the nonprofit Parkinson's Voice Project. So I, I have a landing page for that so you can find someone in your area or your state because of virtual services.
Mark: Right. Yeah. And your website's got really good information there.
Andrea: Thank you
Mark: Some great direction. Like you said by going to your website, I can find somebody here in Arizona that can help and find resources and those things.
So that's fantastic. And your social media, by the way. Very entertaining. You've got some good stuff out there. You've got some stuff that brings up some good education and information. You've also got a lot of fun stuff, so I really do appreciate that.
Andrea: Thank you for those comments. That's so sweet. I'm having fun with it.
I did one that is basically like a slight of hand. I change the scene in a really kind of fast way and now I kind of feel like I have to do that every time, but, I agree with you. I, I try to keep the content really focused on speech therapy or kind of describing the, the things we're talking about here.
Why Speech Therapy Motivates those with Parkinson’s
[00:22:48] Mark: So in looking at your, your repertoire, is there a, a favorite session that you like to do over another? Is, is that a fair question or is there something that you enjoy doing like you look forward to each week or something that, that stands out to you as something I really like.
Andrea: So I would say the evaluation is really fun because I get to like open the door to the other side.
Mark: Right.
Andrea: And they get to like, see it. So that's kind of fun cuz I get to like guide, start guiding them through that and then, ah, it's, I have a, like a program to follow in a way. But I try to be so individualized to the patients. And then also their limitations, if they're having trouble like reading text, or they're really not into reading out loud we're not going to do that.
But one of my client's daughter is going to get married and he's going to do the father of bride speech. And we had to work on that and build up to a, long speech. And just fine tuning, the sequence of events to get to that success, to get to that level.
Some people are really into music. So we talk a lot about music and we do categories of music and describing the music and. You know, a traveling musician is someone I used to work with and like just the stories that they had and the tangents that I could get them on.
And and then challenging them and saying like, oh, I didn't, you know, that wasn't loud enough. Or to being able to kind of clue them in a really direct way. So they can be more successful.
Mark: Well, I was just gonna say it, it, it shouldn't surprise me that somebody that's a speech therapist listens to their people, because that's really what you're telling me.
You meet people, you listen to what they're interested in and, and where they're at. And you tailor it to that. And I really love that because it is individualized sessions. Yeah. But it's also in their wheelhouse. It's something they're interested in. It's that music it's, it's what they're interested in, which helps them be engaged in the, in this therapy. That's fantastic.
Andrea: Absolutely. Yeah. That's that's what, what gets them better,
Mark: Right.
Andrea: If it's motivating to them. They wanna regain back to that meal or to that conversation or to that job again regain their voice and their speech and their swallowing ability. And if they don't have that motivation, they don't see that other end. Then it's, it's hard for me to motivate that.
Mark: Right.
Andrea: And it's, it just been, it's been very, very rewarding to be able to help people. But it's. It's rewarding when I get to meet someone, even another provider or like a physical therapist they don't know the connection of speech and swallowing and Parkinson's disease and I get to spend that moment and discuss that. That happens very often. And I don't want that to be the case. And so I'm, I'm here to support that kind of that change.
Conclusion
[00:25:35] Mark: That's great. This has been an absolute pleasure for me. And I just wanna say having gotten to know you through social media you have been a delight and in the Parkinson's community online, I am finding is very supportive and very engaged.
And though you're not a Parkinson's patient, you are part of the Parkinson's community. It's not just me. A lot of other people out there have felt that support that you have provided in just the inclusion there. So we really do appreciate what it is you offer, but also just being so supportive day to day.
And we really do appreciate it. I know. I appreciate it, Andrea. You're just fantastic. So this has been a pleasure for me.
Andrea: Thank you.
[00:26:13] Mark: And I really do hope that this helps to get word out on how you can help. And if it's not you, like you said, but they can still go to your website and still find assistance.
So maybe once again, what's your website.
Andrea: MyVoiceTherapy.com. And I do wanna say it's been a pleasure speaking with you. I knew it would be, and I knew this would be wonderful. And I know your motivation is to learn for yourself, but also get to get the knowledge out. Thank you. I appreciate you doing this with me.
Don’t worry about sounding professional. Sound like you. There are over 1.5 billion websites out there, but your story is what’s going to separate this one from the rest. If you read the words back and don’t hear your own voice in your head, that’s a good sign you still have more work to do.
Be clear, be confident and don’t overthink it. The beauty of your story is that it’s going to continue to evolve and your site can evolve with it. Your goal should be to make it feel right for right now. Later will take care of itself. It always does.
Contact